What to know about Amyloidosis for USMLE, ABIM, PANCE, ABFM
Amyloidosis is a generic term, defined as extracellular tissue deposition of fibrils composed of low-molecular (light) weight subunits of normal serum protein.
It’s one of those conditions that doesn’t fit neatly into one organ system but here are the things to know about it, as relevant for the ABIM, USMLE, ABFM, and PANCE boards.
The kidneys are often involved with symptoms varying from evidence of slight protein in the urine to nephrotic syndrome. Along with other infiltrative diseases (e.g. sarcoidosis, hemochromatosis), amyloidosis has been shown to cause restrictive cardiomyopathy. The most common EKG finding seen with a patient having cardiac amyloidosis is low voltage. Amyloidosis can also cause secondary autonomic failure and lead to orthostatic syncope, as can diabetes, spinal cord injuries or Parkinson disease.
On biopsy, Congo red staining of the sample yields a characteristic apple green color when viewed under a polarizing microscope.
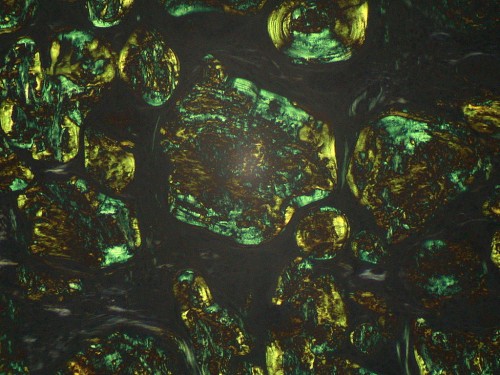
(image from Wikipedia)
Patients who have been diagnosed with amyloidosis should undergo amyloid typing of the deposits to classify the specific amyloidosis present.
There are over 20 low molecular-weight proteins recognized to form myeloid fibrils. Fortunately, for your ABIM, PANCE, ABFM or USMLE exam, you only need to know 2!
AL Amyloidosis
AL amyloidosis is the most common type of amyloidosis. It was the condition previously known as primary amyloidosis. It is one of 4 plasma cell dyscrasias
- Multiple myeloma
- Monoclonal gammopathy of undetermined significance (MGUS)
- Waldenstrom macroglobulinemia
- AL amyloidosis
AL amyloidosis is found in 10% of patients with multiple myeloma.
As above, nephrotic syndrome can be seen in patients with amyloidosis. Other signs that can suggest a diagnosis of AL amyloidosis are:
Skin findings associated with AL amyloidosis are:
- Pinch purpura
- Macroglossia
- Raccoon’s eyes (purpura in periorbital region)
- Waxy skin (scleromyxedema)
Confirmation of a diagnosis of AL amyloidosis is by any of the following:
- Abdominal fat pad aspirate or bone marrow biopsy, revealing apple-green birefringence under polarized light after staining with Congo red
- M protein on serum/urine testing or clonal plasma cells in marrow
The goal of AL amyloidosis treatment is elimination of the monoclonal M protein.
- In carefully selected patients, autologous hematopoietic stem cell therapy (HSCT) is used.
- Those who are not eligible for HSCT may be recommended to undergo chemotherapy. Regimen examples include low-dose melphalan and dexamethasone or bortezomib-based and immunomodulatory therapies.
AA Amyloidosis
AA amyloidosis is a reactivation of another illness/inflammatory process. It is sometimes known as secondary amyloidosis. Serum amyloid A (SSA) protein is an acute phase reactant.
In AA amyloidosis, the most important therapy is to treat the underlying infection or inflammation in order to reduce the level of SAA protein. For instance, AA amyloidosis can arise as a potential long-term consequence of Familial Mediterranean Fever (FMF). As a result, colchicine is given to such patients. With timely, effective treatment of the underlying inflammation amyloid deposits reduce and nephrotic syndrome can improve. However, if the kidney function has become significantly impaired, it rarely recovers.
Although this blog post doesn’t make you an expert on Amyloidosis, it does give you the high-yield information you need for the USMLE, ABIM, ABFM and PANCE boards.
Sources:
MKSAP 17. American College of Physicians.
Board Basics 3. American College of Physicians.
Image: Amyloidosis. https://en.wikipedia.org/wiki/Amyloidosis. Wikipedia. https://upload.wikimedia.org/wikipedia/commons/a/af/Amyloidosis%2C_lymph_node%2C_polarizer.jpg Accessed November 17, 2016.







