USPSTF updates Cholesterol screening guidelines and who should get Statins
General Internal Medicine is commonly covered on USMLE, ABIM, ABFM and PANCE boards. Thus, whenever new clinical guidelines are issued it’s important to know for taking care of patients and exam preparation alike.
New clinical guidelines that potentially increased the number of people who will be prescribed statins topped health headlines last week on the major outlets.
- “New statin guidelines: Everyone 40 and older should be considered for the drug therapy” was the headline in the Washington Post.
- “If you are middle-aged and have even one risk factor for cardiovascular disease, you might need statins to prevent a future stroke or heart attack…” was the opening of a Reuters article.
The media made it seem that there was a very high likelihood that middle-aged patients with just hypertension would be placed on a statin the next time they visited their doctor. That’s not the case.
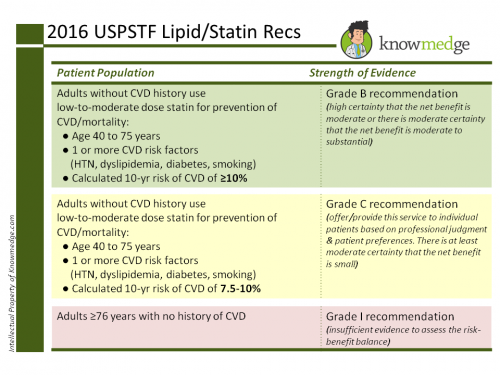
Here’s what the latest guidelines from the United States Preventive Services Task Force (an update to the 2008 recommendations on screening for lipid disorders in adults) concluded, straight from the article in the latest issue of the Journal of American Medical Association.
In brief, a low-to-moderate intensity statin would be recommended for a patient with all of the following :
- 1. Age 40 to 75 years without a history of cardiovascular disease
- 2. At least one risk factor for cardiovascular disease (i.e. dyslipidemia, diabetes, hypertension, or smoking)
- 3. 10% risk of developing cardiovascular disease within the next 10 years
The first two cover a large number of the population in the US, especially when you consider that 70 million American adults have hypertension. However, there are much fewer who would have a 10% risk of developing cardiovascular disease within the next 10 years. In fact, one could argue that a person with such a high risk would be certain to have at least dyslipidemia, diabetes, hypertension or smoking. Therefore, it’s kind of redundant.
How do you calculate the 10-year cardiovascular disease risk?
To calculate the 10-year cardiovascular risk score, the USPSTF recommends clinicians to use the global risk assessment tool developed by the American College of Cardiology (ACC) and the American Heart Association (AHA). The 2013 pooled cohort equations incorporate age, sex, race, cholesterol levels, systolic blood pressure, hypertension treatment, diabetes, and smoking. They can be found here.
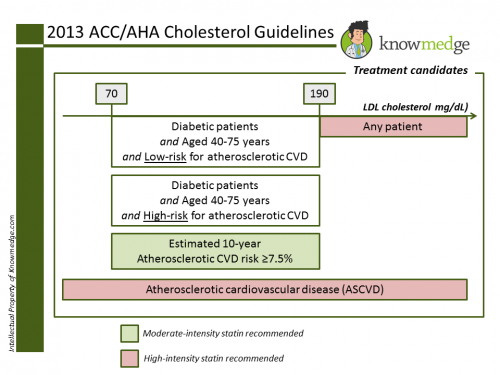
So, how do the latest USPSTF recommendations differ from ACC/AHA cholesterol management guidelines?
Overall, these USPSTF recommendations reinforce the 2013 ACC/AHA recommendations that reduced the importance of hitting a target low-density lipoprotein (LDL) and instead determine the overall cardiovascular risk score.
We’ve detailed those recommendations before:
- USPSTF states that patients with a 7.5-10% risk “may also benefit” from a low-to-moderate intensity statin but did not definitively recommend them. As it’s a grade C recommendation, those patients should have a discussion with the physician about whether or not to start taking a statin.
- Meanwhile, the ACC and AHA recommends that individuals with a 7.5% or greater risk take statins.
What are examples of low-to moderate intensity statins?
Low-intensity statins include the following:
- Simvastatin 10mg daily
- Pravastatin 10-20mg daily
- Lovastatin 20mg daily
- Fluvastatin 20mg daily
- Pitavastatin 1mg daily
Moderate-intensity statins include the following:
- Atorvastatin 10-20mg daily
- Rosuvastatin 5-10mg daily
- Simvastatin 20-40mg daily
- Pravastatin 40-80mg daily
- Lovastatin 40mg daily
- Fluvastatin XL 80mg daily
- Fluvastatin 40mg twice daily
- Pitavastatin 2-4mg daily
What about patients greater than age 75 years?
USPSTF didn’t recommend starting statins in adults greater than age 75 years (making it grade I). They may be continued in patients who are already on them.
References: