What You Need to Know About Transient Ischemic Attacks (TIA) for the ABIM and USMLE Exams
As we close out #NeuroWeek, let’s take a look at Transient Ischemic Attacks (TIA), a diagnosis found within the neurology syllabus of the ABIM and USMLE Step 3 exams. According to the American Heart Association/American Stroke Association, TIA is defined as “a transient neurological deficit resulting from focal brain, spinal cord, or retinal ischemia without acute infarction.”
As you may already know, there really isn’t a”cure” for TIAs. Rather, the objective of admitting a patient experiencing a TIA is to avoid negative outcomes, such as a stroke or death. In fact, about 40% of patients diagnosed with ischemic strokes had a TIA prior to the stroke. Specifically, the first 24-48 hours are a critical timeframe for monitoring for the development of a stroke.
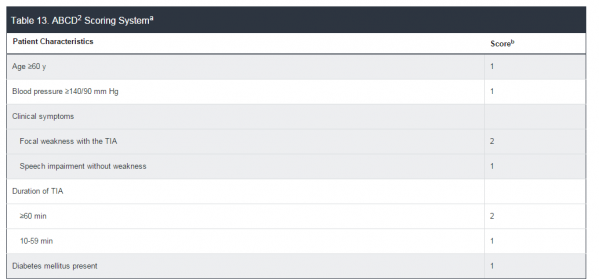
To determine who is at the highest risk of developing complications and thus needs to be admitted (since not every patient diagnosed with a TIA needs to be admitted), we rely on the reliable ABCD2 scoring system. In this risk-stratification methodology, the A stands for Age; B for Blood pressure; C for Clinical presentation; D for Duration of symptoms; and the 2 for the second D: Diabetes mellitus).
- A: Age > or equal to 60: 1 point, Age <60: 0 points
- B: BP>140/90: 1 point, BP<140/90: 0 points
- C: Clinical: Weakness: 2 points, Isolated speech: 1 point, Other: 0 points
- D: Duration: > or equal to 60 minutes: 2 points, 10-59 minutes: 1 point, <10 minutes: 0 points
- D: Diabetes present: 1 point, no diabetes: 0 points
Scores 2 day risk of stroke
- 0-1……….0%
- 2-3……….1.3%
- 4-5……….4%
- 6-7……….8%
If the initial score is 3 or above (or the patient has transient monocular blindness) and the patient presented within the first 72 hours of symptom onset, hospital admission is recommended.
Source: MKSAP 16, American College of Physicians Online. “Neurology: Stroke: Stroke Subtypes: Transient Ischemic Attack.”







