5 High-Yield Gastroenterology Pearls for the ABIM Board & Medical Clerkship Exams
As we mentioned in a previous blog post this week, Gastroenterology and Hepatology comprises about 9% of the ABIM Internal Medicine exam, making it one of the more critical subjects on the boards. Below, we review 5 High Yield Gastroenterology/Hepatology Pearls that may help you score a few extra points on your ABIM or Internal Medicine shelf examination.
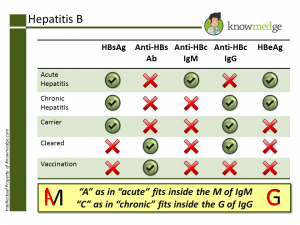
- Interpreting Hepatitis B markers seems like a pain but is worth remembering Start with these key points:
- Hepatitis B surface Antigen (HbsAg) → active infection
- Hepatitis B surface Antibody (HbsAb) → past infection or vaccination against hepatitis B
- Hepatitis Be Antigen (HbeAg) → active replication of the virus
- Anti Hepatitis B core IgM Antibody (Anti-HBc IgM) → acute infection
- Anti Hepatitis B core IgG Antibody (Anti-HBc IgG) → chronic infection
- Chronic → Increased LFTs
- Carrier → Normal LFTs What about that Hepatitis D virus?
- Hepatitis D can’t exist on its own. It requires Hepatitis B infection to be present
- Anti-Hbc IgM + Hepatitis D virus → acute co-infection and will not worsen hepatitis
- Anti-Hbc IgG + Hepatitis D virus → acute super-infection and can cause fulminant hepatitis
- Main causes of dysphagia can be broken down into Mechanical & Motility Problems
- Intermittent problem
- Esophageal ring (AKA as Steakhouse Syndrome)
- Clue in history: Patient has difficulty swallowing while chewing foods like bread or steak.
- Long standing history of GERD
- Barrett’s esophagus (squamous to columnar metaplasia) or stricture formation.
- Dysphagia to solids with significant weight loss
- If long standing smoking history, Squamous cell carcinoma more likely
- If long standing history of uncontrolled GERD, Adenocarcinoma more likely
- Eosinophilic esophagitis
- Dense eosinophilic infiltrate into the epithelium of the squamous epithelium
- Mainstay of treatment is viscous budesonide, fluticasone, or proton pump inhibitors (PPIs)
- Intermittent and associated with chest pain, especially after drinking carbonated drinks
- Diffuse Esophageal Spasm (DES)
- Associated with connective tissue disease or heartburn
- Scleroderma
- Associated with cough/regurgitation with improvement of dysphagia with raising hand above the head
- Achalasia (which can be associated with Chagas Disease)
- Before treating with surgical myotomy or pneumatic dilatation, EGD must be done first to rule out secondary achalasia from lymphoma or cancer.
- Achalasia will have increased LES tone on manometry studies. GERD, on the other hand, will have decreased LES tone.
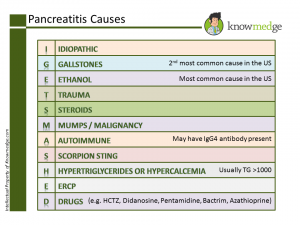
- Remember the main causes of Pancreatitis by the mnemonic “I GET SMASHED”
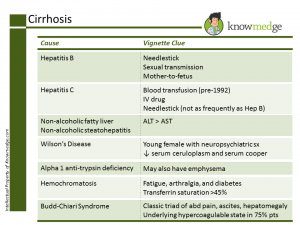
- Alcoholics aren’t the only folks to develop cirrhosis To the lay public, cirrhosis is to alcohol as lung cancer is to smoking. However, we know that it’s not such a simple association. Smokers aren’t the only patients to develop lung cancer and those who don’t drink alcohol can still become cirrhotic. Let’s review some of the non-alcohol related causes of liver failure with two easy-to-digest slides:
- They may both be considered IBD, but know how to distinguish Ulcerative Colitis and Crohn’s Disease Ulcerative Colitis
- Presents with abdominal pain and bloody diarrhea that is chronic
- Problem starts in the rectum and spreads proximally (backwash ileitis)
- Pathology reveals superficial ulcers with crypt abscesses
- Some common extra-intestinal manifestations include:
- Aphthous ulcers
- Pyoderma gangrenosum
- Primary sclerosing cholangitis
- Ankylosing spondylitis
- Arthritis (mirrors Ulcerative Colitis)
- Erythema nodosum (mirrors Ulcerative Colitis)
- Can show positive p-ANCA on labwork
- Colonoscopy should be done 8 years after diagnosis and then every 1-2 years afterwards as patients with UC have an increased risk of colon cancer
- If dysplasia is seen on colonoscopy, total proctocolectomy should be performed
- Rectum is spared with Crohn’s Disease. Crohn’s Disease occurs mainly in the terminal ileum (Skip lesions are common)
- Common presentation is right lower quadrant mass, weight loss, and diarrhea (can be bloody but can also be watery)
- Pathology will show deep ulcers with granuloma formation
- Not as common to see extra-intestinal manifestations with Crohn’s Disease as is seen in patient with UC
- Colon cancer can occur but is more common in UC patients
- Can show positive ASCA (anti-Saccharomyces Cerevisiae antibodies) on labwork
- Colonoscopy should be done 8 years after diagnosis and then every 1-2 years
- If dysplasia is seen on colonoscopy, total protocolectomy should be performed
 (Click above image to view larger size)
(Click above image to view larger size)
As you see above: Along with the Cleared state, both Chronic and Carrier Hepatitis B patients will have positive HBsAg and Anti-HBc IgG. How can these two conditions be differentiated? Easily. Just look at the Liver function tests (LFTs)
- Mechanical Problems (dysphagia to solids first and liquids later)
- Motility Problems (dysphagia to both solids and liquids concurrently)
 (Click above image to view larger size)
(Click above image to view larger size)
First, we review Viral Hepatitis, Fatty Liver/Steatohepatitis, Wilson’s, Alpha 1 Anti-Trypsin Deficiency, Hemochromatosis and Budd-Chiari along with helpful clinical clues that may appear in the question vignette:
 (Click above image to view larger size)
(Click above image to view larger size)
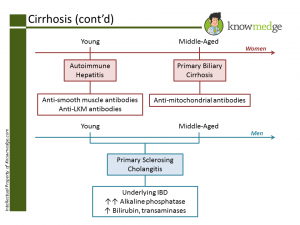
Of course, we can’t forget Autoimmune Hepatitis, Primary Biliary Cirrhosis, and Primary Sclerosing Cholangitis. Many medical students and residents find it confusing to match up the gender, age, and serologies with the correct condition. While these are not hard-and-fast rules, for exam purposes, in general we can use the following colorful schematic to make it tough to ever forget again.
 (Click above image to view larger size)
(Click above image to view larger size)
The above 5 pearls should help reinforce important concepts you may encounter in the gastroenterology content of the ABIM or Medical Clerkship exams.







