5 Must-Know Eye Conditions for the ABIM Board and NBME Shelf Exams
While most of the ABIM Examination topics fall neatly into organ system categories, not all of them fit into this schematic. These include: ophthalmology, primary care screening guidelines, vaccinations, etc. Here at Knowmedge, we’ve incorporated this important group of subject areas into General Internal Medicine, similar to the American College of Physicians’ Internal Medicine In-Training Exam Blueprint.
Today, in this first of a series of blogs, we review the key eye diseases: Conjunctivitis, Macular Degeneration, Glaucoma, Retinal Detachment, and Cataracts. The eyes may see only what the mind knows, but your mind should know these eye conditions for the ABIM exam. The exam is several months away so go ahead and bookmark this page so you can quickly review it once more in the days before you obtain your certification or recertification.
1. Conjunctivitis
Conjunctivitis is broken down into viral, bacterial, and allergic conjunctivitis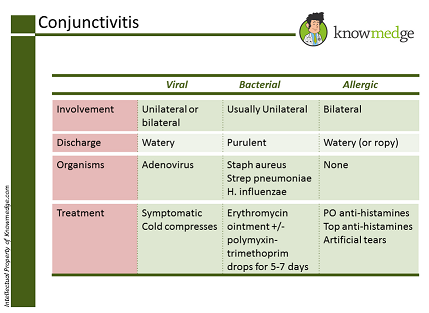 Viral
Viral
- Usually caused by adenovirus
- Having a preceding upper respiratory infection or recent exposure to a person with conjunctivitis are clues to aid in the diagnosis
- Acute onset
- Usually unilateral redness
- Watery discharge is present
- Highly contagious
- Frequent hand washing must be performed to prevent spread of infection
- Supportive treatment including cold compresses and artificial tears. NO role for antibiotic eye drops with viral conjunctivitis
Bacterial
- Common causing agents are Staph aureus, Streptococcus pneumoniae, or Haemophilus influenzae. People who wear contact lenses can be infected by Pseudomonas aeruginosa
- Presence of mucopurulent discharge and crusting can occur in the morning when the discharge is dry
- Usually leads to redness of unilateral eye but may have bilateral involvement if spread occurs by rubbing both eye
- Should be treated with antibiotics (e.g. erythromycin ointment and/or polymyxin-trimethoprim drops) for 5-7 days
- Patients who wear contact lenses should not wear contact lenses for at least 7 days
- If patient has bacterial conjunctivitis for 4 weeks, this is chronic in nature and should be evaluated by an ophthalmologist
Allergic
- Can mimic viral conjunctivitis in terms of having clear (or ropy) discharge but predominant symptom is eye itching that corresponds to specific seasons
- Treatment is with oral anti-histamines, topical anti-histamines, and artificial tears
For another look at conjunctivitis, take a look at our previous post
2. Macular Degeneration
- Common in elderly individuals
- Can lead to visual loss
- Progression of disease can lead to difficulty reading, driving, or performing activities of daily living
- Two sub-types of macular degeneration are dry (atrophic) and wet (neo-vascular). Most cases are dry macular degeneration. If, however, patient has wet macular degeneration, it is more serious and can lead to blindness in an acute fashion rather than progressive fashion.
- Biggest risk factors are age, family history, cardiovascular disease, and smoking
- Quitting smoking reduces the risk of developing macular degeneration and some studies suggest that diet high in anti-oxidants can be protective. Patients can also benefit by using a magnifying glass.
3. Glaucoma
Condition is a condition resulting from increased intra-ocular pressure due to blockage in drainage of aqueous humor. It can be broken down into primary open angle glaucoma (POAG) and acute angle closure glaucoma.POAG
- Most common form of glaucoma and most common cause of irreversible blindness in the world
- Painless loss of peripheral vision that is gradual in nature. Later on it can affect central vision
- Optic cup: disc ratio >0.5
- Risk factors include age greater than 40, being African-American race, and positive family history
- Mainstay of treatment is with pharmacological eye agents such as beta blockers, carbonic anhydrase inhibitors, adrenergic agonists, hyperosmotic agents, and prostaglandin analogues
- More severe than POAG
- Red eye, severe pain, headache, nausea and vomiting and visual halos
- Intra-ocular pressure can be as high as 50 mm Hg
- When suspected, immediate referral to an ophthalmologist is required to prevent permanent optic nerve atrophy
4. Retinal Detachment
- Patients may present with floaters, squiggly lines, flashes of light
- This is an ophthalmology emergency and requires immediate attention by an ophthalmologist
5. Cataracts
- Opacity of lens will occur
- Symptoms include painless decreased visual acuity, decreased night vision, glare, and sometimes double vision
- Physical examination can reveal a decreased or absent red reflex
- Treatment is surgical removal of the cataract
Once again, the folks who write the Internal Medicine licensing exams don’t expect you to have the depth of knowledge regarding the plethora of eye diagnoses that an ophthalmologist possesses. However, topics such as the ones mentioned in the pearls above should assist you with the General Internal Medicine section of the med school clerkship shelf, ACP in-training and ABIM board exams.








[…] of Physicians’ Internal Medicine In-Training Exam Blueprint. Earlier this week, we reviewed the 5 key eye diseases seen on the ABIM board and NBME shelf exams. Today we explore the high-yield topic of […]