What to know about the 2017 ACC/AHA Hypertension guidelines for USMLE, ABIM, ABFM, PANCE, etc
Like cholesterol guidelines, blood pressure guidelines are an essential part of the daily work of all physicians. While primary care physicians are often the ones who provide initial counseling and treatment, monitoring a patient’s blood pressure is a responsibility of every doctor who interacts with that patient. As home blood pressure monitors become easier to use and become capable of integrating with electronic medical records, all physicians will be presented with even more blood pressure data at each patient encounter. Expect to see it on the various boards, including the USMLE, ABIM, ABFM, and PANCE.
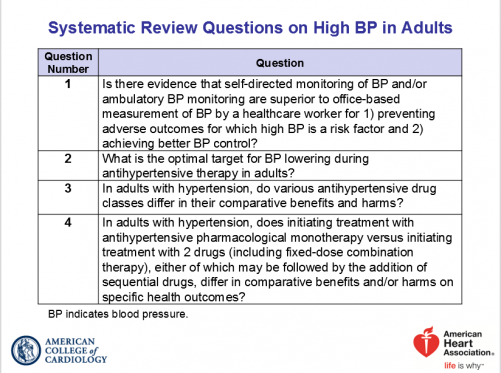
The American College of Cardiology/American Heart Association and others who helped draft the guidelines had the following objectives:
Understanding the latest blood pressure guidelines will help you in your clinical practice as well as your preparation for the USMLE, ABIM, PANCE, ABFM, etc. Blood pressure is a reliable predictor of the likelihood of developing heart attacks and strokes. As stated in the New York Times piece on the blood pressure guidelines, only smoking is a stronger preventable cause.
Note that these guidelines from the American College of Cardiology and American Heart Association haven’t been accepted across all specialities but should still start to appear on exams soon.
What are the main numbers to remember?
The threshold for labeling hypertension dropped from 140/90 mmHg to 130/80 mmHg. As a result, the U.S. adult prevalence of hypertension now increases from 32% to 46%.
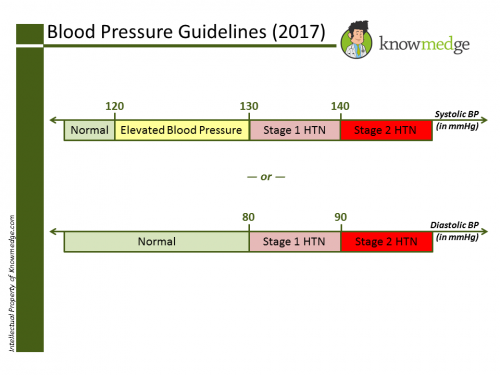
So what’s considered prehypertension now?
Prehypertension is no longer part of the blood pressure guideline lexicon. Instead, the term is now “elevated blood pressure.” It’s defined as a systolic pressure of 120-129 mmHg with a normal diastolic pressure, up to 80 mmHg.
The new guidelines don’t just talk numbers, but also about how to capture blood pressure data.
It emphasizes incorporating out-of-office blood pressure measurements using validated devices, given the commonly encountered phenomenon of white coat hypertension. This also captures cases of masked hypertension in which the patient’s blood pressure in the medical office is normal but elevated at home.
Are there separate guidelines for the elderly?
The 2014 BP guidelines (JNC 8), which were known as the JNC 8, had a different cut-off for older people, which was at 150 mmHg. Now, there is no difference based on age. As a result, an individual aged 65 or older will be recommended to bring down their blood pressure to 130/80 mmHg or less using both lifestyle and medication. Medication is urged because simply being 65 or older places the individual at above the 10% cardiovascular disease threshold for pharmacotherapy.
What about those with kidney disease or diabetes?
They too will have the same 130/80 mmHg cut-off.
Now that we know who to consider having elevated blood pressure and who to call hypertensive, how do we treat these conditions?
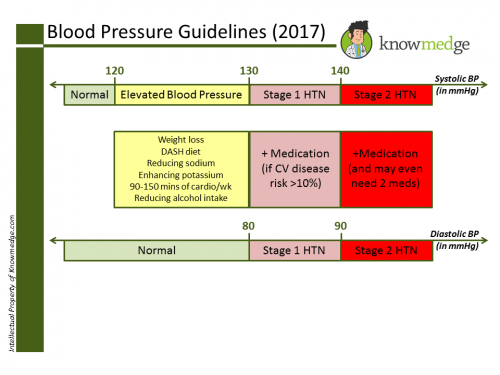
For those with elevated blood pressure—meaning a blood pressure between 120 and 129 mmHg—lifestyle intervention solely is the recommended treatment. This entails six goals:
- Weight loss
- DASH diet
- Reducing sodium
- Enhancing potassium
- 90 to 150 minutes of cardiovascular exercise weekly
- Reducing alcohol intake
Hypertensive patients with a blood pressure between 130 and 139 mmHg—meaning those with stage 1 hypertension—should also undergo the above lifestyle interventions. In addition, they may benefit from pharmacological treatment if their 10-year cardiovascular disease risk (based on the ACC’s cardiovascular risk calculator) exceeds 10%. Keep in mind that this is the same risk calculator used in evaluating high cholesterol. The guidelines state that if the patient “has already had a cardiovascular event such as a heart attack or a stroke…medication should be prescribed.” While that’s true, you don’t need to necessary remember this redundant point since those folks will have a greater than 10% risk based on the ACC calculator.
Who should be screened for secondary hypertension?
Boards love to check if you’re too quick to do a secondary hypertension workup. Therefore, restrict the workup to only those with the following conditions:
- Drug-resistant or drug-induced hypertension
- Abrupt onset of hypertension
- Onset less than 30 years of age
- Abrupt onset/worsening of hypertension
- Target organ damage *
- Malignant hypertension
- Diastolic hypertension for pts 65 years and older
- Excessive hypokalemia
* Target organ damage defined as: Cerebrovascular disease, hypertensive retinopathy, left ventricular hypertrophy, left ventricular dysfunction, heart failure, coronary artery disease, chronic kidney disease, albuminuria, peripheral artery disease
Feel free to share your thoughts in the comments section below. Your insight may even help others studying for the USMLE, ABIM, ABFM and PANCE boards.
Sources:
- New ACC/AHA High Blood Pressure Guidelines Lower Definition of Hypertension. Published November 13, 2017.
- 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report From the Panel Members Appointed to the Eighth Joint National Committee (JNC 8) Paul A James, Suzanne Oparil, Barry L Carter, et al. Journal of American Medical Association. Published February 5, 2014.
- Kolata, Gina. ”Under New Guidelines, Millions More Americans Will Need to Lower Blood Pressure.” New York Times. Published November 13, 2017.








October 13, 2023
This is the most successful gaming project https://ragingbull.bet/ in my memory! Such a rapid growth of the service is worthy of respect. Thanks to bonuses to the depu, I’ve been swimming in money for six months, thanks to Raning Bull