Topic Refresher: Medical Management of Stable Angina Pectoris
Stable angina pectoris–the presence of chest pain/pressure/discomfort that arises with exertion and resolves with rest–is the most common manifestation of coronary artery disease (CAD).
Managing stable angina requires a combination of lifestyle modification to reduce risk factors (e.g. smoking cessation, weight management, daily cardiovascular activity, diet improvement, and co-existing diabetes/hypertension/hyperlipidemia) as well as anti-anginal medical therapy.
The key mechanism of anti-anginal medications is to vasodilate the coronary vasculature and decrease oxygen demand by the myocardium, thus reducing the frequency and severity of anginal episodes and improving quality of life. Secondary prevention medical treatment prevents future cardiovascular events such as heart attack and stroke.
Here are the key tips for medically managing stable angina pectoris for both the wards, as well as your medical board exam, including USMLE, ABIM, ABFM, and PANCE.
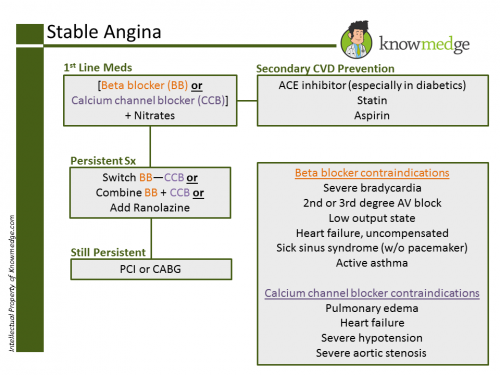
1) Offer either a beta blocker or a calcium channel blocker as first-line treatment for stable angina.
Decide which drug to use based on comorbidities, contraindications and the person’s preference. (see image above for details)
2) If the person’s symptoms are not satisfactorily controlled on a beta blocker or a calcium channel blocker, consider either switching to the other option or using a combination of the two.
Do not routinely offer anti-anginal drugs other than beta blockers or calcium channel blockers as first-line treatment for stable angina.
Do not routinely offer a third anti-anginal drug to people whose stable angina is controlled with two anti-anginal drugs.
Do add a third anti-anginal drug only when:
- the person’s symptoms are not satisfactorily controlled with two anti-anginal drugs and
- the person is waiting for revascularization or revascularization is not considered appropriate or acceptable.
Offer a short- or long-acting nitrate for preventing and treating episodes of angina. Advise people with stable angina:
- how to administer the short-acting nitrate
- to use it immediately before any planned exercise or exertion
- that side effects such as flushing, headache and light-headedness may occur
- to sit down or find something to hold on to if feeling light-headed.
- to repeat the dose after 5 minutes if the pain has not resolved
- to call the paramedics if the pain has not gone 5 minutes after taking a second dose.
- long-acting nitrates can be in oral tablet pill form (e.g. Isosorbide dinitrate, Nitroglycerin SR) or applied transdermally (e.g. Nitropaste) or applied under the gums (Nitrogard). Isosorbide mononitrate has a longer half-life (4-6 hours) than isosorbide dinitrate. Side-effects include headache and lightheadedness. These side-effects generally wear off. If they do not, notify your physician. When taking Nitrates, avoid overly hot showers and baths as this may make you dizzy and fainting is possible. To prevent dizziness, get up slowly from a sitting or lying position.
For people on beta blocker or calcium channel blocker monotherapy whose symptoms are not controlled and the other option (calcium channel blocker or beta blocker) is contraindicated or not tolerated, consider adding ranolazine.
Review the person’s response to treatment, including any side effects, 2–4 weeks after starting or changing drug treatment. Titrate the drug dosage against the person’s symptoms up to the maximum tolerable dosage.
Do not offer vitamin or fish oil supplements to treat stable angina. Inform people that there is no evidence that they help stable angina.
3) Consider revascularization (coronary artery bypass graft [CABG] or percutaneous coronary intervention [PCI]) for people with stable angina whose symptoms are not satisfactorily controlled with optimal medical treatment.
Offer CABG to people with stable angina and suitable coronary anatomy when:
- symptoms are not satisfactorily controlled with optimal medical treatment AND
- revascularization is considered appropriate AND
- PCI is not appropriate
Offer PCI to people with stable angina and suitable coronary anatomy when:
- their symptoms are not satisfactorily controlled with optimal medical treatment AND
- revascularization is considered appropriate AND
- CABG is not appropriate
When either procedure would be appropriate, explain to the person the risks and benefits of PCI and CABG for people with anatomically less complex disease whose symptoms are not satisfactorily controlled with optimal medical treatment. If the person does not express a preference, take account of the evidence that suggests that PCI may be the more cost-effective procedure in selecting the course of treatment.
When either procedure would be appropriate, take into account the potential survival advantage of CABG over PCI for people with multivessel disease whose symptoms are not satisfactorily controlled with optimal medical treatment and who: have diabetes or are over 65 years or have anatomically complex three-vessel disease, with or without involvement of the left main stem.
Ensure that there is a regular multidisciplinary team meeting to discuss the risks and benefits of continuing drug treatment or revascularization strategy (CABG or PCI) for people with stable angina.
The team should include cardiac surgeons and an interventional cardiologist.
4) If the person cannot tolerate beta blockers and calcium channel blockers or both are contraindicated, consider ranolazine
Decide which drug to use based on comorbidities, contraindications, the person’s preference and drug costs.
5) Drugs for secondary prevention of cardiovascular disease
Cardioprotective medications not only reduce cardiovascular events and the progression of systemic atherosclerosis but also improve survival.
- Consider aspirin (at least 75mg daily) for people with stable angina, taking into account the risk of bleeding and comorbidities
- Add angiotensin-converting enzyme (ACE) inhibitors for people with stable angina and diabetes
- Offer moderate-to-high intensity statin treatment for lipid modification
- Offer treatment for high blood pressure in line with Hypertension